In enterprise systems, reliability starts with a clean, normalized data model centered around a core object. Classic examples are a customer in a CRM like Salesforce, or an employee in an HRIS like Workday. For an EMR in healthcare, that object is the patient. A patient-centered EMR schema establishes a single source of truth which simplifies scaling, maintenance, and system logic.
In Canvas, we’ve named this concept our Deep Unified Architecture. What this means to us, and our customer, is a unified system spanning the relational database, application logic, and developer interfaces. Every object is versioned, linked with strong referential integrity, and exposed through our SDK which enables precise control, safe customization, and high developer velocity.
What Is Deep Unified Architecture?
Canvas’s Deep Unified Architecture leverages standard ontologies to ensure that every piece of clinical, financial and operational data is semantically meaningful and interoperable.
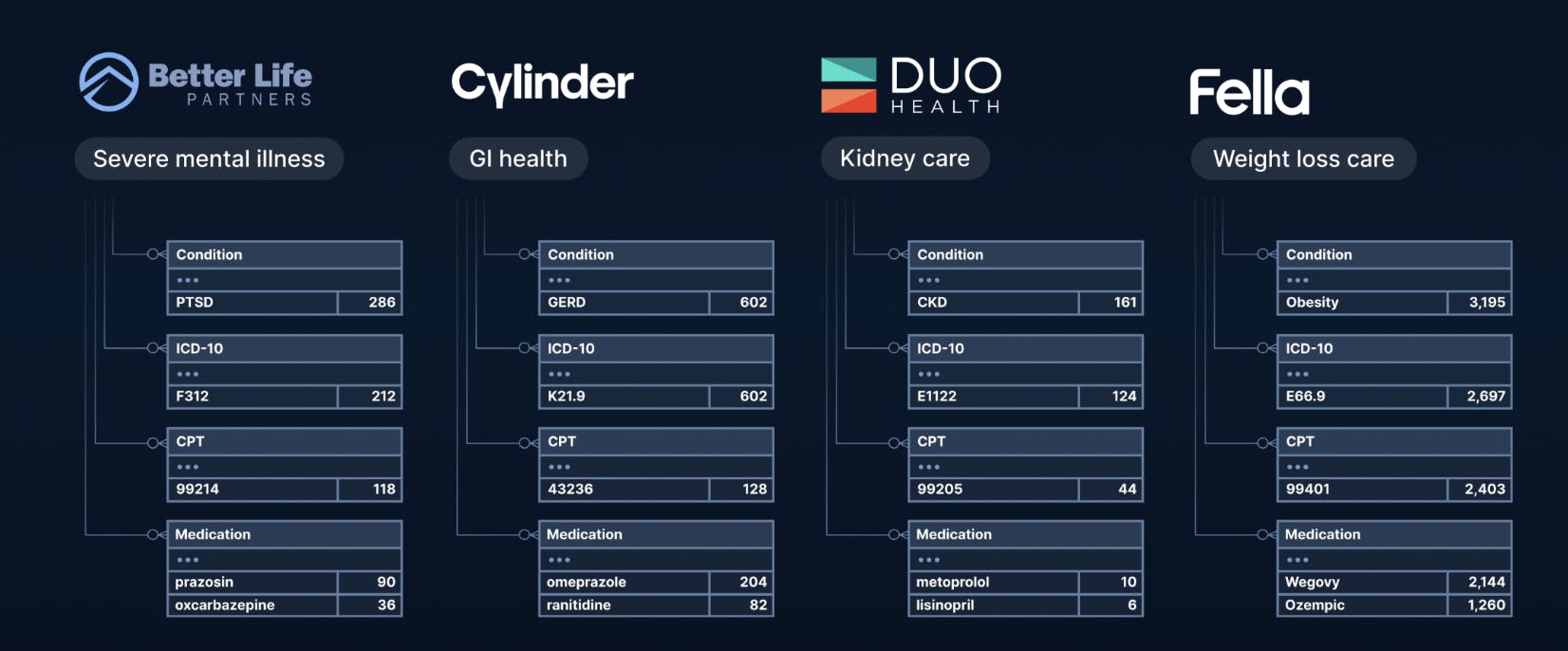
Canvas structures data using widely accepted medical coding systems—not only for labeling and storage but also to power intelligent search, retrieval, and clinical workflows:
- LOINC (Logical Observation Identifiers, Names, and Codes): Used for lab tests and clinical measurements. For example, a blood glucose test is coded as LOINC 2345-7. Our ontology synonyms enable a clinician to search "blood sugar" and immediately retrieve all relevant lab results, regardless of how the test was originally named by different labs.
- ICD-10 (International Classification of Diseases, Tenth Revision): Used for diagnoses. For instance, essential hypertension is coded as I10. This standardization allows systems to surface related patient cohorts (e.g., all patients with hypertension) quickly and accurately during clinical decision support or population health reporting.
- CPT (Current Procedural Terminology): Applied to procedures and services. A flu vaccine administration is coded as 90686. Ontology-driven search ensures that related procedures—like different flu vaccine types—can be automatically added or retrieved without needing users to memorize exact codes.
- HCC (Hierarchical Condition Categories) and RAF (Risk Adjustment Factor): Employed for risk adjustment in value-based care models. For example, diabetes with chronic complications (ICD-10 E11.22) maps to HCC 18. By enhancing our data with links to HCC, Canvas can not only support accurate billing but also dynamically surface gaps in documentation during clinical workflows.
By linking these ontologies with our data model, Canvas improves both the write cycle (ensuring data is structured and codified correctly at the time of entry) and the read cycle (enabling faster, more precise queries and workflow automations without relying on brittle keyword matches).
How Canvas Developer Tools Leverage Deep Unified Architecture
The Canvas Software Development Kit (SDK) includes several modules, like the Events, Effects, Handlers, Commands, Data, and Utilities modules, that together allow developers to customize and extend the EMR. At the core of this system is the Data Module, which provides direct access to the Deep Unified Architecture, enabling developers to interact with the complete, structured clinical and operational record. This unified data access allows other SDK modules to create clinical protocols, automate workflows, define routing logic, and customize forms — all based on a consistent, standards-driven data foundation.
Data Module
Canvas structures clinical data using widely accepted medical coding systems like ICD-10, LOINC, CPT, and HCC — but its real differentiator is how the Deep Unified Architecture links these domains into a coherent, fully navigable model. Through the Data Module, developers gain curated, secure access to both Protected Health Information (PHI) and non-PHI, representing the real-time state of the Canvas instance.
The Data Module provides convenience methods and operators that make complex business and clinical logic easy to express. Rather than pulling isolated records, developers can easily move across conditions, labs, procedures, encounters, clinicians, and billing — enabling sophisticated, real-time applications that would require expensive custom integrations or overnight reporting in traditional EMRs.
For example:
- You can find patients whose chronic disease is poorly controlled, and immediately see whether the right follow-up was scheduled and by whom — without needing to manually piece the information together. Example: retrieve all diabetic patients (ICD-10 E11.9) whose most recent HbA1c test (LOINC 4548-4) is above 9%, identify if a follow-up visit (CPT 99214) was scheduled within 30 days, and surface the responsible provider and location — all through a single, streamlined query.
- You can automatically identify patients who are missing important care, directly tied to both their clinical conditions and risk adjustment needs, without running separate reports. Example: build real-time panels that combine risk adjustment and clinical care gaps, such as finding patients with an HCC category for COPD (HCC 111) who have not had a spirometry test (LOINC 19868-9) in the past 12 months, seamlessly linking diagnoses, observations, and procedure histories.
- You can trigger outreach programs based on missed quality measures the moment they happen, with full clinical context immediately available to the care team. Example: automatically flag patients for care management outreach if a hospitalization (inpatient encounter type) lacks a documented transition of care visit (CPT 99495 or 99496) within 14 days, with immediate access to the original admission diagnosis and discharge labs.
Because these relationships are modeled natively, not bolted on, Canvas offers critical advantages that traditional EMRs cannot match:
- Precise, clinically grounded workflows: Developers can combine specific conditions, labs, procedures, providers, and encounters in a single query to power real-world use cases.
- Fluid movement across data domains: Canvas makes it possible to seamlessly connect clinical, operational, and financial data — from diagnosis to lab to visit to bill — without manual stitching or reconciliation.
- Operational timing and automation: Developers can easily build time-sensitive workflows (like follow-ups within 30 days or post-discharge care within 14 days) that trigger in real time, not after a nightly batch.
- Seamless developer experience: Built for fast queries with no fragile ETL pipelines and no backend dependencies — just intuitive access to a deeply interconnected clinical model.
This foundation enables the creation of deeply context-aware, highly responsive applications that legacy systems simply cannot support.
Why Deep Unified Architecture is Essential for Autonomous Agents in Healthcare
As healthcare moves towards automation, the need for systems that can support autonomous agents becomes critical. Canvas’s architecture is designed with this future in mind:
- Real-Time Context: Agents can access up-to-date patient information, enabling timely interventions.
- Read/Write Capabilities: Using the Canvas SDK, agents can retrieve and update records, place orders, and modify care plans.
- LLM Integration: The platform supports integration with multiple large language models, allowing agents to interpret and generate clinical, operational and financial documentation.
- Autonomous Operation: With structured data and robust APIs, agents can operate within the EMR, performing tasks like scheduling, documentation, and patient communication autonomously.
- Processing Speed: Agents leverage the Deep Unified Architecture to retrieve, reason over, and act on patient data quickly enough to support real-time workflows in clinical settings.
Legacy systems lack a complete or semantically coherent data model, and do not have server side SDKs to use the data for context and then modify user interaction or automate workflows. This forces them to operate, in effect, blindfolded and with two hands tied behind their backs.
Workarounds like copy/paste from third-party apps or robotic process automation (RPA) add cost, complexity, and risk — while limiting the impact agents can have on clinical operations. Instead of enabling real clinical transformation, these workarounds often constrain agents to low-value, clerical tasks.
By exposing the full structured record through its Deep Unified Architecture, Canvas removes these barriers and enables agents to operate intelligently, efficiently, and autonomously inside the EMR itself.
Conclusion
By embracing standard ontologies and enabling developers with unmatched capabilities, Canvas accelerates everyday medicine into the future where autonomous agents enhance care delivery and improve outcomes.
To explore the Canvas platform, developers can get hands-on with the Canvas Developer Sandbox and review the Canvas SDK documentation. If you are part of a care delivery organization interested in how Canvas can support your clinical or operational goals, contact our team to learn more.